The Prior Authorization Process Flow Chart: A Step-by-Step Guide
Navigating the prior authorization process can be challenging for both patients and providers. Whether you're waiting on an approval for a prescribed medication or preparing for a scheduled medical procedure, understanding the steps involved is essential.
Prior authorization—also referred to as prior auth, preapproval, or precertification—is a process that health insurance companies use to determine whether a specific treatment, medication, or medical service is medically necessary and covered under a patient’s insurance plan.
To help clarify what happens behind the scenes, we’ve outlined a simplified prior authorization process flow chart that illustrates how a typical request moves from submission to decision. This flow chart showcases the role careviso plays in this process.
What Is a Prior Authorization Flow?
Prior authorization is a coverage review conducted before certain services or prescription drugs can be provided. It applies to many health insurance plans, including Medicare Advantage plans, commercial insurers, and Medicaid services. A prior authorization request is a prerequisite for many types of care as required by the No Surprises Act.
This process is intended to confirm the medical necessity of a treatment and ensure it aligns with the insurer’s clinical guidelines. Without verifying prior authorization eligibility, patients may be responsible for the full cost of care.
The following flow chart breaks down each phase of the process.
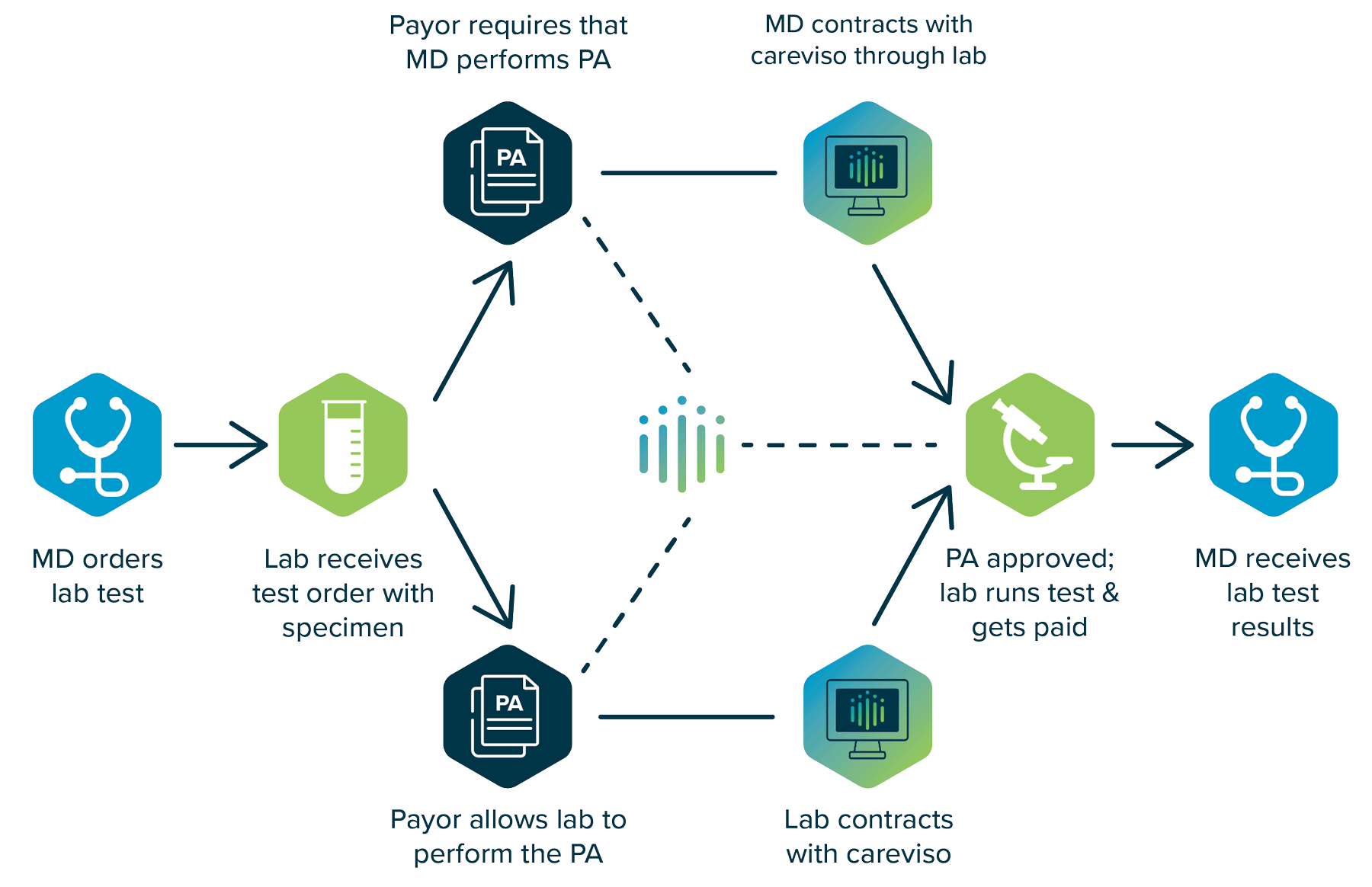
The PA process begins with the doctor ordering lab tests. The lab receives the test order with the specimen. From there, the prior authorization process can go one of two ways:
A. If the insurance company allows the lab to perform the prior authorization, the lab contracts with careviso to send the prior authorization request and get it approved.
B. If the insurance provider requires the doctor to carry out the prior auth, the doctor will sign a BAA with careviso, who performs the prior authorization request on their behalf.
Once prior authorization approval is provided for either option, the lab will then run their testing, receive payment, and send the lab test results to the doctor.
Why the Prior Authorization Flow Chart Matters
A clear prior authorization process flow chart can help healthcare providers anticipate next steps, reduce delays, optimize their revenue cycle management, and improve communication with payers. It also helps patients better understand why certain services take time to schedule or why clinicians require additional information.
Where Delays Can Occur in Prior Authorization
Even when following the process correctly, PA request delays can still occur due to:
- Incomplete or inconsistent documentation
- Variations in prior authorization requirements across payers
- Lack of real-time benefit data
- Manual submission methods such as fax or phone
- Staffing limitations in healthcare provider offices
These challenges are particularly common in practices managing large volumes of Medicare Advantage enrollees, prescription medication requests, or specialty treatments.
READ MORE: How Long Does Prior Authorization Take?
How Digital Tools Improve the Prior Auth Process
Electronic prior authorization (ePA) solutions like careviso’s seeQer platform help modernize and streamline the prior authorization process. By integrating directly into healthcare provider workflows and electronic health records (EHRs), digital tools can:
- Provide real-time eligibility and benefit checks
- Identify required prior authorization up front
- Accelerate submission and response times
- Reduce manual errors and claim denials
With automation, a healthcare provider can spend less time on administrative tasks and more time focusing on patient care.
READ MORE: careviso Achieves 2 Million Prior Authorizations
How careviso Helps
careviso’s technology platform, seeQer, is built to simplify and accelerate the prior authorization process. By offering real-time insights into health insurance company requirements, out-of-pocket costs, and prior authorization approvals, careviso helps healthcare providers make faster, more informed decisions at the point of care.
For practices dealing with complex authorizations—whether for medication, imaging, or surgery—seeQer helps reduce the risk of prior authorization denial, supports efficient medical billing, reduces administrative burden for providers, and increases overall patient satisfaction.
As the healthcare system evolves, a more transparent and connected approach to prior authorization is not only possible but necessary. With tools like seeQer, healthcare providers can navigate the process more confidently and patients can receive the care they need without unnecessary delay.
Discover how seeQer informs patients and transforms practice.
Schedule a seeQer demonstration of benefits verifications, cost assessments, and other essential tasks in the platform. Learn how seeQer can help your organization reduce administrative burden, transform cumbersome processes, and provide transparency that empowers patients in a complex and ever-changing industry.